Case History
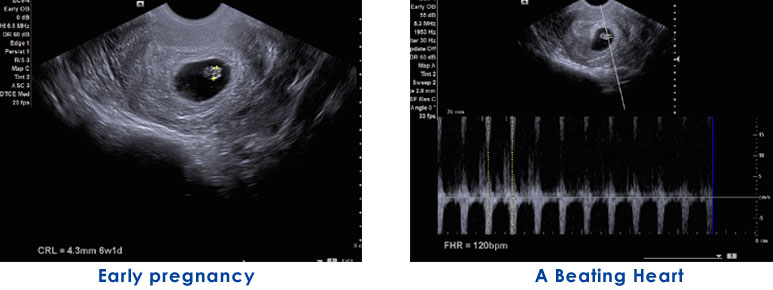
This is a case of a 32 years old lady, presenting at 12 weeks of gestation for a routine Level I scan (Nuchal Scan). Her previous scan at 8weeks showed a normal sized foetal pole with normal cardiac activity. She had a history of hypothyroidism for which she was on Tab Thyronorm 75/100mcg od. She had history of two previous miscarriages at 6-8weeks of gestation, first a chemical pregnancy and second an anembryonic pregnancy.
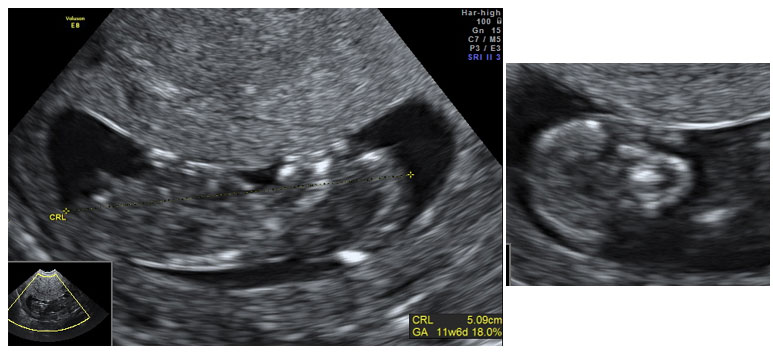
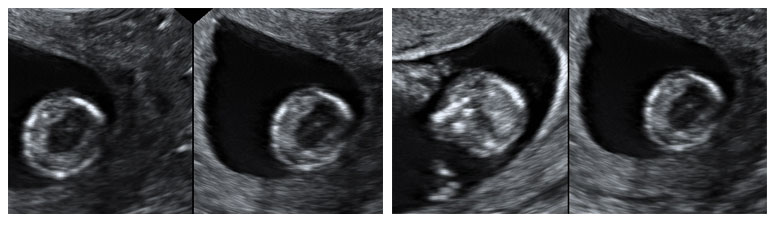
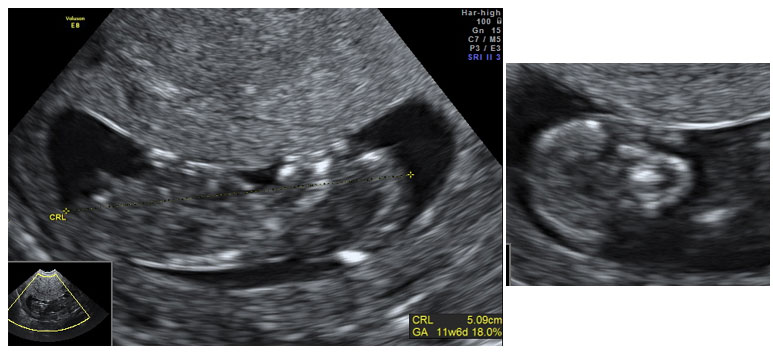
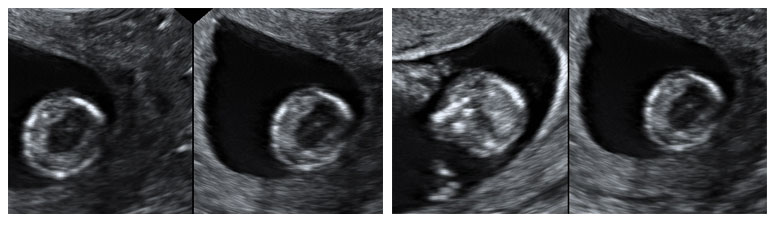
The present Level I scan revealed a small cranium with a monoventricle (absence of the butterfly appearance of chorod plexus). The cerebrum appeared to be fused anteriorly. The posterior fossa appeared normal for the gestational age.The orbital and nasal structures could not be delineated. Rest of the fetal body was unremarkable. The nuchal lucency was around 1.0mm. Ductus venosus showed normal forward flow. My final diagnosis was of Holopresencephaly (semilobar type) with craniofacial abnormalities.
The lady presented a few days later with bleeding and signs of inevitable abortion.
Discussion
Holoprosencephaly refers to absent or incomplete division of the prosencephalon and is the most frequent malformation of the prosencephalon. There is incomplete division of the prosencephalon during the fourth and eight week of gestation. Its incidence is 1 in 16,000 and 1 in 250 spontaneous abortion.
It is classified into 3 types according to the degree of cerebral involvement: alobar, semilobar and lobar. The clinical features vary depending upon the severity of holoprosencephaly.
- Alobar is the complete absence of division of the prosencephalon structures, resulting in complete absent interhemispheric fissure, corpus callosum, fused thalami and only oncerebral ventricle and facial dysmorphism. It is the most lethal.
- Semilobar, consisting in incomplete separation of cerebral hemispheres, connected in the frontal area, with a singular ventricular cavity and a partially fused thalami.
- Lobar, consisting of interhemispheric fissure, absent septum pellucidum and frontal horns communicate freely. Corpus callosum is normal or hypoplastic . It is the least severe form.
Another variant, the Middle Interhemispheric type has also been described.
The etiology of holoprosencephaly includes genetic and environmental factors. Environmental causes include maternal diabetes mellitus, alcoholism, inutero infections like CMV, rubella, toxoplasma, drugs like retinoic acid and cholesterol synthesis inhibitors. It can be transmitted in an autosomal dominant way. Mutation of SHH gene is the most frequent cause of familial holoprosencephaly. It is also asscoicated with Trisomy 13.
Prenatal diagnosis of holprosencphaly includes ultrasonography, fetal MRI, cytogentic analysis and molecular analysis of fetal DNA.
Prognosis is dependant on the degree of fusion and malformation of the brain as well as other health complication. Children born with lobar holoprosencephaly can survive for a few years but develop various neurological deficits.